Pacemaker Clinic
What is a Pacemaker?
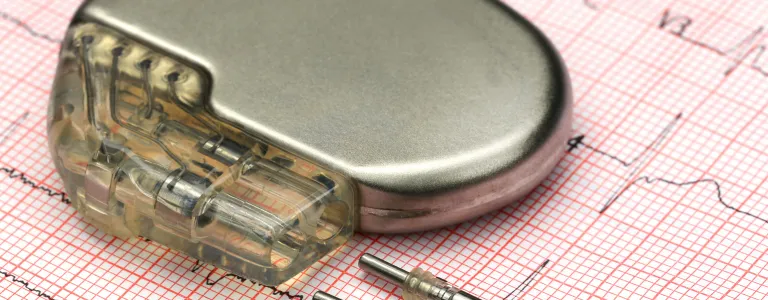
A pacemaker is a small, battery-operated medical device implanted in the chest or abdomen to help regulate abnormal heart rhythms. It sends electrical impulses to the heart to ensure it beats at a normal rate and rhythm. Pacemakers are most often used to treat bradycardia (a slow heart rate) but can also be used for other heart rhythm issues. The device consists of two parts: a pulse generator, which houses the battery and the electronics, and leads (wires) that deliver the electrical impulses to the heart.
Who Needs a Pacemaker?
A pacemaker is typically recommended for individuals with heart rhythm disorders, particularly those who have a slow or irregular heartbeat. Some conditions that may require a pacemaker include:
- Bradycardia: A condition where the heart beats too slowly, leading to dizziness, fatigue, and fainting.
- Heart Block: A condition where the electrical signals between the upper and lower chambers of the heart are delayed or blocked.
- Atrial Fibrillation (AFib): In some cases, patients with irregular and fast heart rhythms may benefit from a pacemaker if medications do not control the heart rate adequately.
- Heart Failure: Pacemakers, especially specialized types like biventricular pacemakers, can be used to help improve the pumping efficiency of the heart in patients with heart failure.
Pacemakers are generally recommended when the heart’s natural pacemaking system is not working correctly and causing symptoms such as fatigue, dizziness, or fainting.
Types of Pacemakers
There are several types of pacemakers, each designed to address specific heart rhythm problems:
- Single-Chamber Pacemaker: This type has one lead placed in either the right atrium or right ventricle of the heart. It helps control the rhythm of either the upper or lower chambers of the heart.
- Dual-Chamber Pacemaker: This type has two leads, one in the right atrium and one in the right ventricle. It helps coordinate the timing between the upper and lower chambers of the heart, improving efficiency.
- Biventricular Pacemaker (Cardiac Resynchronization Therapy - CRT): This is used for people with heart failure. It has three leads placed in the right atrium, right ventricle, and left ventricle, helping the heart's chambers beat in sync.
- Rate-Responsive Pacemaker: This pacemaker adjusts the heart rate based on your activity level, ensuring that the heart beats faster during exercise and slows down at rest.
How is a Pacemaker Procedure Done?
The pacemaker implantation procedure is minimally invasive and typically done under local anesthesia. Here’s a step-by-step overview:
- Preparation: The patient will be given a local anesthetic to numb the area where the pacemaker will be implanted, usually just below the collarbone. In some cases, mild sedation may also be given.
- Incision: A small incision is made near the collarbone, and the leads (wires) are guided through a vein into the heart using X-ray guidance.
- Lead Placement: The leads are positioned in the appropriate chambers of the heart. They are then connected to the pacemaker device, which is inserted under the skin near the incision.
- Testing and Adjustment: Once the pacemaker is in place, the doctor will test the device to ensure it’s functioning correctly and adjust the settings if needed.
- Closure: The incision is closed with stitches, and the patient is usually discharged within a day or two.
What Precautions Should Be Taken After a Pacemaker is Installed?
After receiving a pacemaker, it is important to take certain precautions to ensure proper functioning and avoid complications:
- Activity Limitations: Avoid lifting heavy objects or raising your arm on the side of the pacemaker above shoulder level for several weeks after the procedure to allow the leads to settle in place.
- Medical Device Interference: Keep a safe distance from strong electromagnetic fields, such as MRI machines, industrial equipment, and certain electronics, as they may interfere with the pacemaker's function. Always inform healthcare providers about your pacemaker before undergoing any procedure.
- Follow-Up Appointments: Regular follow-up appointments are crucial to monitor your pacemaker’s battery life and performance. Your doctor will adjust the settings if necessary.
- Monitor for Symptoms: If you experience dizziness, fainting, palpitations, or unusual fatigue, notify your doctor immediately, as these could indicate that your pacemaker needs adjustment.
- Carry a Pacemaker ID Card: Always carry identification that you have a pacemaker, in case of emergencies.
- Avoid Direct Impact: Protect the area around the pacemaker from direct physical trauma, such as from contact sports.
